Pancreatitis in Dogs
The pancreas is an important organ that lies on the right side of the abdomen, adjacent to the stomach and the duodenum (upper part of the small intestine). The pancreas has two main jobs. Firstly, it secretes digestive enzymes to break down food. Secondly it secretes the hormones insulin and glucagon, to help regulate blood sugar.
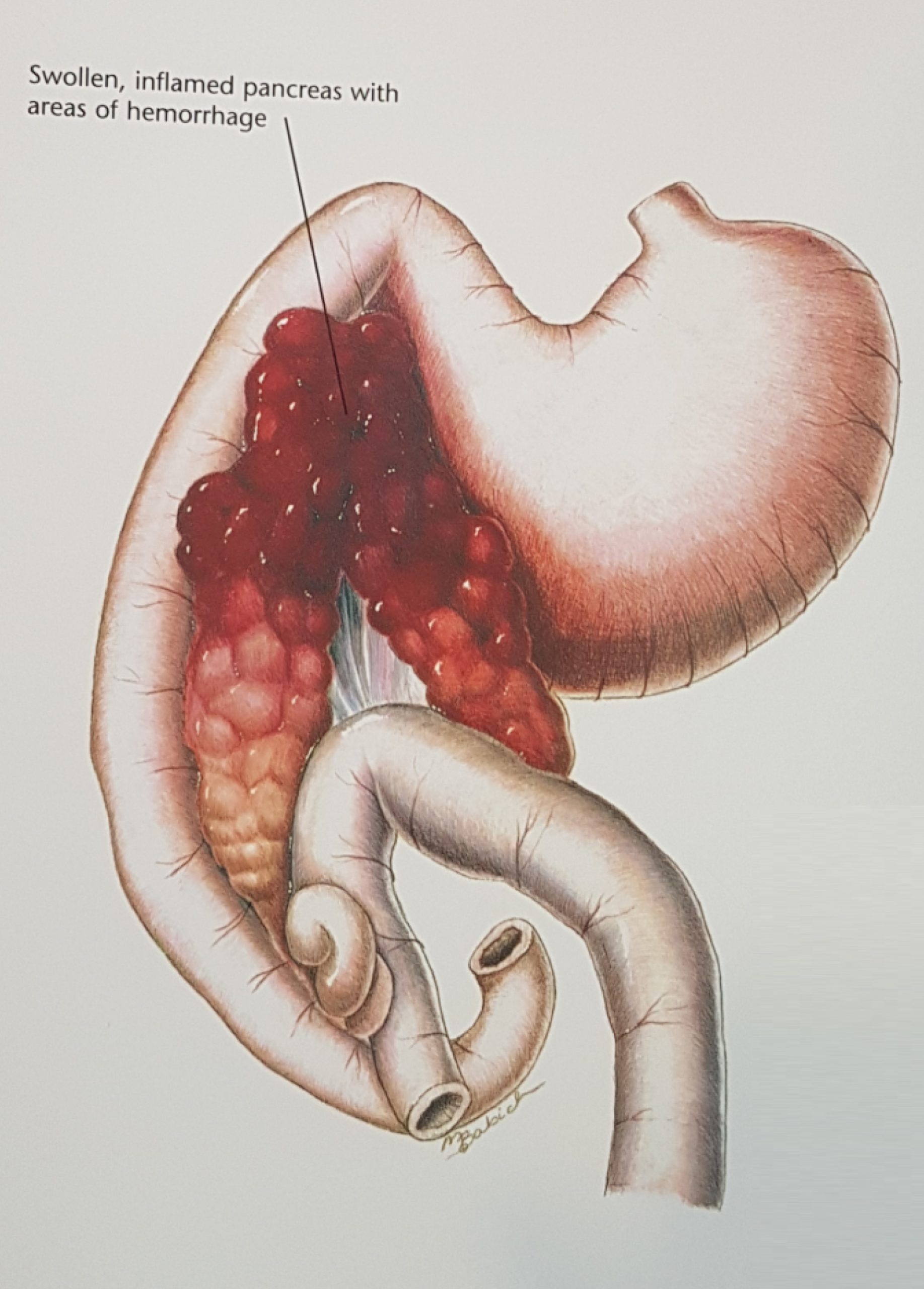
Image taken from Hills’s Atlas of Clinical Anatomy
Pancreatitis is a common condition that occurs in dogs in Singapore. Pancreatitis is due to inflammation of the pancreas, and can be acute, chronic, or acute on chronic. This inflammation disrupts the normal integrity of the pancreas. Digestive enzymes, normally stored safely as inactive forms, are prematurely activated and released internally, digesting the pancreas itself and nearby organs such as the liver. Toxins released from this tissue destruction can result in kidney and liver injury, Systemic Inflammatory Response Syndrome (SIRS), Disseminated Intravascular Coagulation (DIC) and Acute Respiratory Distress Syndrome (ARDS). Diabetes mellitus can result when the pancreas is damaged, disrupting its ability to produce insulin.
Signalment and Causes

Pancreatitis can occur in any breed of dogs, although certain breeds such as Miniature Schnauzers, Yorkshire Terriers, Silky Terriers and Miniature Poodles may be at increased risk of developing pancreatitis. Middle aged to older dogs who are overweight also appear to have a higher risk.
In most cases, we do not find the exact cause of pancreatitis. However, the known possible causes of pancreatitis are:
- A sudden fatty meal is the classic cause of pancreatitis.
- Hyperlipidemia (high levels of triglycerides and cholesterol in the blood). Miniature Schnauzers are predisposed to hyperlipidemia and pancreatitis.
- Several medications such as azathioprine, potassium bromide and L-asparaginase have been implicated as causes of pancreatitis.
- Hormonal conditions such as hypothyroidism, diabetes mellitus, hyperadrenocorticism (Cushing’s disease).
Clinical signs and History
The common symptoms of pancreatitis are decreased appetite or anorexia, vomiting, diarrhea, lethargy, fever and abdominal pain. In severe cases, the dogs may become depressed, or present in acute hypovolemic shock.
Diagnosis
Pancreatitis is usually diagnosed based on the history, clinical signs, and a combination of blood tests and an abdominal ultrasound scan. A complete blood count often shows an elevated white blood cell count. Blood levels of the pancreatic enzymes lipase and amylase can be high in pancreatitis, but these tests are not very sensitive or specific in diagnosing pancreatitis.
The Idexx SNAP cPL (Canine pancreas-specific lipase) test is a more accurate blood test for diagnosing pancreatitis. This test measures canine lipase levels specific to the pancreas, and takes less than 30 minutes to run in the clinic. An abnormal result is highly suggestive of pancreatitis. However, an abnormal result can sometimes be due to other causes, such as small intestinal foreign body obstruction.
Abdominal ultrasonography is much better at diagnosing pancreatitis than abdominal x-rays. An ultrasound scan may show an enlarged hypoechoic pancreas, with signs of inflammation in the surrounding mesentery. One study of pancreatitis showed that ultrasonography was able to detect 68% of cases. Ultrasound also allows assessment of other abdominal organs, and collection of fluid from the abdomen for analysis. A normal ultrasound does not rule out pancreatitis.
Treatment
There are no specific treatments for pancreatitis. The most important parts of supportive care are rehydrating the patient to restore circulation to the pancreas, and providing pain and nausea medication to keep the patient comfortable, restore appetite, and prevent further dehydration.
Mild cases can be treated with outpatient treatment. These dogs are given subcutaneous fluid therapy, oral medications (anti-vomiting, antacid, painkillers), and are usually given a low fat bland diet eg Hill’s I/D Low Fat diet, or a home cooked diet of boiled chicken/fat-free cottage cheese and steamed rice, split into multiple small meals a day.
Moderate cases may require hospitalization with intravenous fluid therapy, potassium supplementation, injectable medications and placement of a temporary feeding tube.
Antibiotics are not usually indicated in pancreatitis. However, severe cases with shock, fever, diabetes mellitus or evidence of breakdown of the gastrointestinal barrier may require prophylactic broad-spectrum antibiotics.
Severe cases eg. those with pancreatic abscesses or biliary obstruction, may require surgical intervention. Those that develop SIRS or DIC will require aggressive supportive care (eg colloid therapy and fresh frozen plasma transfusion) in the hospital.
Prognosis
The prognosis depends on the severity of the disease when first diagnosed and the response to initial therapy. Mild to moderate cases have a good prognosis. Severe pancreatitis is associated with a guarded prognosis, especially dogs that present with shock and depression. These cases can lead to euthanasia because of the cost of hospitalization and intensive care, or because of multi-organ failure, sepsis, SIRS or DIC.
Long Term Consequences
Some patients may have chronic pancreatitis or recurrent intermittent bouts of acute pancreatitis that require long-term management, especially with a low fat diet.
Permanent damage to the pancreas can result in exocrine pancreatic insufficiency (EPI), where the pancreas does not produce adequate digestive enzymes. These dogs will need long term daily enzyme supplementation.
Some dogs may also develop diabetes mellitus and require daily insulin administration to manage blood glucose levels.